Kenya’s Health ministry has tasked the National AIDS and STI Control Programme (NASCOP) to oversee the national roll out and implementation of the three test HIV testing algorithm transitioning from a two-test algorithm that will ensure that correct and timely HIV diagnosis is achieved by maximizing the likelihood of correctly determining one’s HIV status as the countrie’s HIV prevalence falls.
According to Head of National Aids and STI control program (NASCOP) Dr Rose Wafula, the transitioning to a three-assay HIV testing algorithm which will now require three consecutive reactive tests to provide an HIV positive diagnosis is expected to limit the risk of misdiagnosis given the now low number of individuals living with HIV in Kenya who do not know their status.
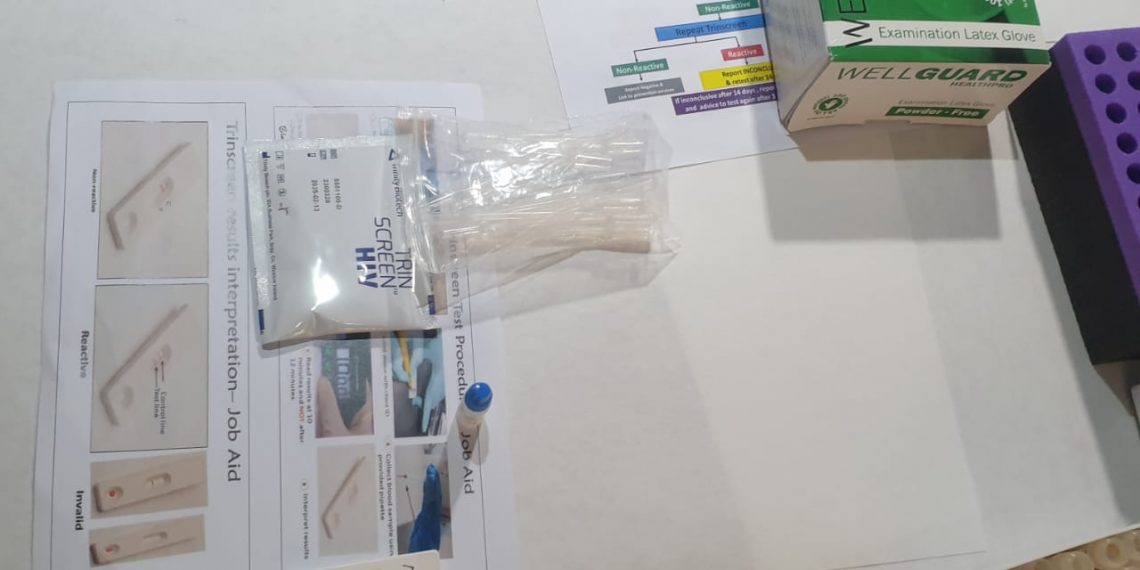
Dr Rose explained that the three test HIV testing algorithm which will include an initial rapid test (RDT) and two confirmatory tests -3-test algorithm- is expected to ensure 99 percent positive predictive value (PPV) is achieved changing the way people used to be diagnosed with HIV.
She added that the adoption of the 3-test HIV testing algorithm will ensure that the risk of a misdiagnosis (false negative or false positive) is reduced to an absolute minimum.
“With the evolution of global HIV epidemiology, HIV testing approaches must also evolve to maintain accuracy and efficiency in population-level diagnosis, NASCOP is also pushing for newer and better tools guided by scientific evidence for HIV response,” Dr Rose Wafula said, adding that, “The three-test HIV testing algorithm rollout begins the first week of July in the Keny’s ASAL counties and it will be strategically and seamlessly done to avoid interruption of ongoing services.
She added that, Kenyans testing for HIV will now have their blood samples tested on three different test kits that work in slightly different ways. In the three-test strategy, you can only be told you have HIV after three consecutive reactive (positive) tests.
“If you are told that you are HIV positive or negative after the three tests, you can be confident that is the case,” Dr Rose said.
“World Health Organization (WHO) recommended a shift to three-test algorithm for countries with a HIV prevalence of less than 5percent with Kenya’s prevalence standing at 4.3percent the three test algorithm will ensure quality services as the country move towards ending AIDs in 2030 and for children by 2027 and achieve the UNAIDS 95-95-95 targets, Dr Rose explained adding that “The WHO guidance also highlights the need to introduce dual HIV/syphilis rapid diagnostic tests (RDTs) and to phase out older testing technologies.”
According to WHO false HIV test results can happen, although they are rare. This is why more than one test is needed to diagnose HIV. To avoid situations where people are misdiagnosed with HIV, WHO is encouraging countries with HIV prevalence below 5percent such as Kenya to increase the number of tests that are used to confirm an HIV diagnosis. By making this change, countries will be able to ensure HIV testing remains accurate, even as prevalence continues to decline.
A false-positive diagnosis has important consequences for individuals (the psychosocial impact of an HIV diagnosis, the health implications of unnecessary ART, public health consequences (the substantial costs of lifelong ART and related services for misdiagnosed people) and damage to the reputation of and trust in the HIV program.
According to Nascop, Kenya conducted a thorough review of the current two -test HIV testing algorithm through a taskforce formed in March 2022 compromising of Ministry of health officials, researchers and technical partners and the evidence from the technical taskforce recommended adoption of the 3-test algorithm based on its sensitivity and specificity.
The taskforce was charged with reviewing performance reports of the current HIV testing algorithm and available evidence to adapt the three-test algorithm as per WHO recommendation. It was also to contextualize the adaption process and advice on the implementation.
The report revealed sufficient evidence indicating that the two-test algorithm was not optimal for HIV testing in the country especially guided by latest data from the Kenya Population -based HIV Impact Assessment (KENIPHIA) revealing that 2018 HIV prevalence stood at 4.9 percent with great subnational variation from <0.1 percent in Garissa county to a high of 19.6 percent in Homabay county, with the national prevalence declining to 4.3 percent in 2021 according to National Aids Control Council (NACC 2021).
According to Medical Services Principal Secretary Harry Kimtai, As of December 2023, over 1.3 million PLHIV were under treatment across 3,752 facilities nationwide. Annually, Kenya conducts more than 8 million HIV tests across 8,851 testing sites, demonstrating the nation’s commitment to standardized and accessible testing services.