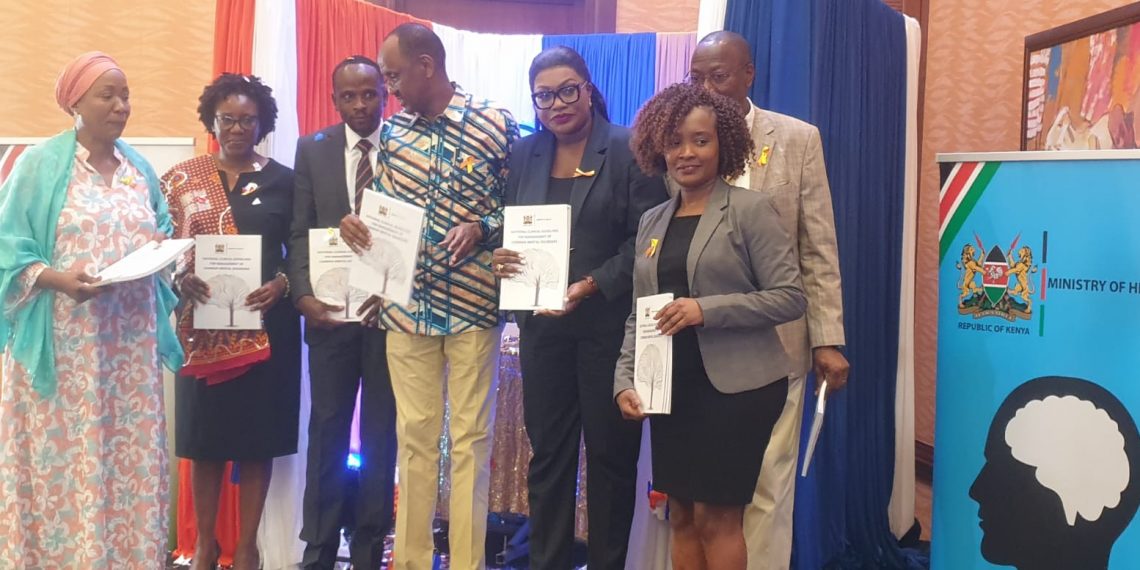
Ministry of Health has unveiled new national clinical guidelines designed to enhance the management of common mental health disorders.
Dr. Patrick Amoth, Director General of the Ministry of Health, emphasized the urgent need for these guidelines.
“Mental disorders remain among the top ten causes of disease burden worldwide, and there has been no significant global reduction since 1990. In Kenya, about 42 percent of individuals seeking care in primary health facilities exhibit symptoms of severe depression, with common mental disorders such as depression and anxiety affecting approximately 10.3 percent of the population,” Dr. Amoth stated. He highlighted that mental health literacy among primary healthcare workers is low, contributing to a significant treatment gap estimated at 75 percent.
The new mental health guideline launch was held in conjunction with World Suicide Prevention Day and is a key step toward improving mental health care accessibility and quality across the nation.
The new guidelines aim to standardize the assessment and management of prevalent mental health conditions, including depression, anxiety, and psychosis. They provide a systematic approach to diagnosis, treatment, and referral, addressing special considerations for populations such as the perinatal period, older adults, and those with co-occurring physical conditions.
“This comprehensive approach will guide healthcare workers through a multidisciplinary framework, ensuring better patient care,” Dr. Amoth added.
Dr. Mercy Karanja, Acting Head of the Division of Mental Health, described the launch as a milestone.
“This guideline is a major step forward in improving access to mental health services in Kenya. It will help standardize care and bridge gaps in treatment,” she said.
Dr. Isaak Bashir, Acting Director of the Directorate of Family Health, urged practitioners to adhere to the new guidelines.
“While these guidelines are crucial, they are not a substitute for further training and should be used in conjunction with other policy documents and technical guidelines,” Dr. Bashir noted.
In addition to the guidelines, Kenya also introduced the WHO Mental Health Gap Action Programme (mhGAP) adapted to the local context.
The mhGAP aims to scale up services for mental, neurological, and substance use disorders in low- and middle-income countries. The intervention guide addresses nine critical areas, including PTSD, anxiety disorders, and substance use disorders, with the goal of providing care even in resource-scarce settings.
Despite these advancements, mental health care in Kenya remains relatively inaccesible,inconsistent and inadequate with wide human resource gap.
Additionally, stigma and discrimination associated with mental health problems are barriers to the health seeking behaviors of persons living with a mental health condition.
Mental health cases has been on the rise affecting millions of individuals.It is estimated that one in every ten people has a common mental health disorder with 25percent of outpatients and 30 percent of inpatients having a mental health condition.