Kenya is fast-tracking plans to build a local vaccine industry, aiming to sustain childhood immunisation and strengthen health security as the country transitions from international support.
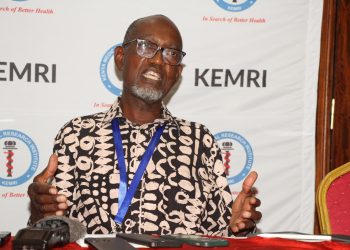
Speaking at the 16th Kemri-Annual Scientific and Health (KASH) Conference, Dr. Ernest Wandera, research scientist at the Kenya Medical Research Institute (KEMRI) and leader of the Kemri vaccine research team, outlined a three-phase strategy to ensure the country can meet national and regional vaccine demand.
The first phase, “fill and finish,” imports bulk vaccine antigens from licensed manufacturers for local packaging and distribution. Childhood vaccines are the priority, as Kenya prepares to graduate from Gavi, the global vaccine alliance that has co-financed immunisation programmes.
“The fill and finish phase ensures our immunisation programmes continue seamlessly once Gavi support ends,” Wandera said.
The second phase will establish a “smart vaccine facility” at Konza Technopolis, allowing end-to-end local production through technology transfer from Korean partners. Initial targets include typhoid conjugate and pneumococcal conjugate vaccines, with plans to expand production over time.
The third phase focuses on research and development, led by KEMRI and local universities. Vaccine candidates for priority diseases such as malaria, rotavirus, Shigella, and cholera will be developed and scaled up by Kenya Biovax for mass production.
Kenya is also establishing an mRNA vaccine platform with support from the World Health Organization, which will enable locally developed vaccines against emerging diseases and future health emergencies.
Quality assurance is central to the strategy. The Pharmacy and Poisons Board oversees vaccine regulation and secured WHO maturity level 3 certification to meet international standards, allowing procurement by organizations like UNICEF.
The National Quality Control Labs also monitors vaccine quality, with ongoing efforts to strengthen capacity.
Wandera noted that market access remains a key challenge, as neighbouring countries may still rely on Gavi support. Officials are engaging partners early and exploring continent-wide coordination through the African Union to avoid duplication and ensure vaccines reach countries that need them.
Construction of the fill and finish facility by Kenya Biovax in Embakasi is underway, with enabling infrastructure like water and sewer lines complete.
Wandera estimates the facility will be ready by 2027, with the first locally produced vaccines available by 2028.
“Local vaccine manufacturing is essential to prevent disruptions in immunisation programmes, ensure health security, and support economic growth,” he said. “These facilities create jobs and strengthen pharmaceutical sovereignty.”
Wandera hope Kenya’s push to become a regional vaccine hub will secure national health needs and advance African self-reliance in critical public health interventions.