Thalia Psychotherapy, an organisation specializing in building tools that in the long run will help in addressing mental health challenges is on the move.
After a successful launch in Nairobi and adjacent areas recently, now it’s headed down to the counties.
Information obtained from the organisation shoes that it’s re-designing it’s portable scream therapy room in a bid to make it accessible by rural communities.
The organisation’s Behavioural Innovation Lead, Maryann Anyango revealed that Thalia is prototyping smaller, head-only units to widen coverage across Kenya’s workplaces, campuses, clinics, and retail corridors. Prototyping is the process of creating a tangible, early version of a product, service, or system to test a concept.
“We built a friendly first step into mental health—simple, measurable, and judgment-free,” she said about a concept that’s gaining ground in Kenya so quickly.
A scream you can measure. Kenyan business leaders admit, and are putting prevention at the front door of care. They want to safeguard the health of their customers, employees and in turn increase productivity.
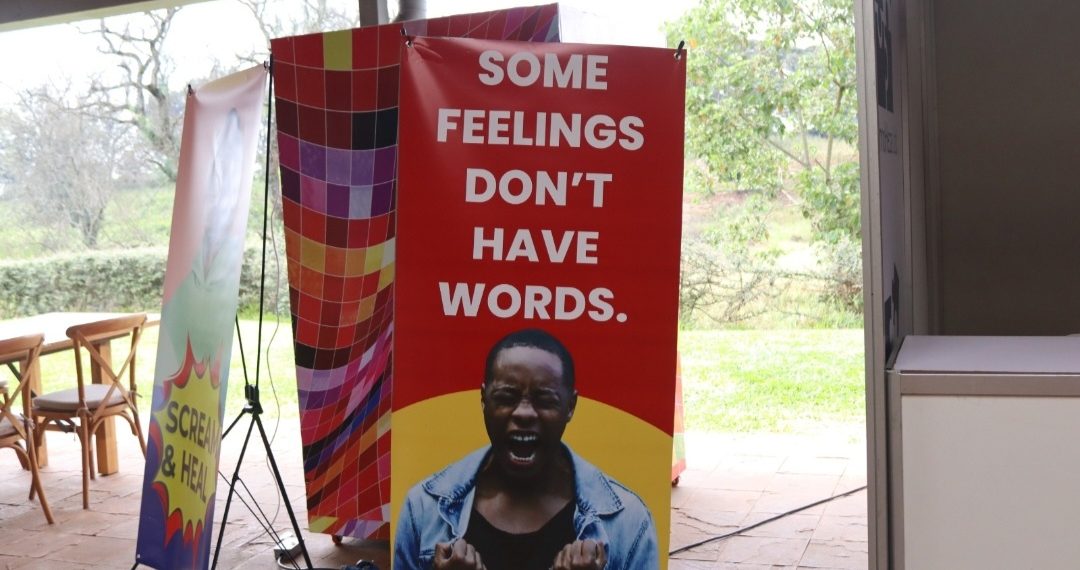
Last week, the organisation unveiled its portable Scream Therapy Room during the 3rd edition of the Transforming African MedTech Conference (TAMC)—a modern, voice-guided booth that lets employees “let go” safely in 12 seconds, visualizes the release, and translates the peak decibels into familiar Kenyan sound references.
It’s playful on the surface and serious in intent, Anyango states, and advises that this is a sure way of making mental health tangible, stigma-free, and a true entry point to care for staff and customers.
“You hear your own power, you see
your progress, and you leave with a nudge toward healthier habits.” Anyango said, outlining how the booth folds into employer benefits and community activations.
For leaders watching benefit costs climb, the timing matters. Medical insurance remains one of the toughest lines in general insurance—frequently a loss-making class—while sector analyses
show rising pressure on claims and loss ratios across the market.
Recent industry reporting notes medical insurance as a leading loss maker and highlights elevated loss ratios, underscoring why pure “curative” cover is getting pricier for employers.
A prevention-first layer can bend that curve, Anyango says.
Kenya’s own mental-health investment case estimates the economy lost Sh62.2 billion in 2021 to mental health conditions—lost productivity, absenteeism, and care costs that compound inside companies.
Global research and regional public-health briefs also connect unmanaged stress, alcohol misuse, and other behavioural risks with higher Non Communicable Diseases (NCDs) burden—costs that ultimately show up in medical claims and performance.
The booth is designed to slot into three channels; employer programs via Mindful Kenya, where staff can access sessions as part of a capitated, prevention-focused bundle; insurer-integrated wellness, adding a measurable behavioural touch point to plans that are often weighted toward treatment rather than prevention.
“For employees, the value proposition is practical: a short, guided release; a neutral, tech-forward experience that feels more like a voice assistant than a clinic; and personalized nudges that link
everyday stress to healthier coping, instead of pathways like heavy drinking, comfort eating, or chronic sleep loss that drive long-run risk,” she said.
For employers, it is a gateway that increases engagement with care earlier, supports safer coping at scale, and supplies anonymized insight on usage patterns—without prying into individual health data.
Thalia says its first production unit was capital-intensive to build—largely due to the AI engine and UX—but scale manufacturing will push unit costs down sharply as the hardware commoditizes.
The strategic point for decision-makers is simple: make mental health the front door, not the back office.
A prevention layer that people actually use—because it’s quick, dignified, and a little bit fun—nudges risk down before it turns into high-cost claims and lost output.
With employer healthcare spending under pressure and medical loss ratios stubbornly high, that shift is more than optics; it’s operational common sense.